Let the Healing Begin
Our Mission
To provide free surgical and dental services to poor and underprivileged children and young adults in various countries throughout the underdeveloped world, as well as facilitate the transfer of education, knowledge and recent innovations to the local medical communities.
Medical Missions for Children, Inc.,(MMFC) is a Massachusetts based non-profit organization that dispatches teams of volunteer surgeons, anesthesiologists, dentists, nurses, speech pathologists, and nutritionists to the most remote and underprivileged communities in the developing world. The focus of MMFC’s missions is the surgical care of cleft lip and palate deformities, head and neck tumors, severe burn injuries, microtia(absence of the outer ear), and dental disease. As well, we work to advance medical education and clinical training, and to expand hospital care facilities, in every country we visit.
Every year, MMFC completes twenty to twenty-five medical missions at multiple sites in eleven different countries. Volunteer teams vary from five and fifteen members, and over the course of one to two weeks, care is provided to between 40 and 300 children and families.
.

Since 1991, MMFC has launched 520 volunteer missions worldwide, providing surgical, dental, rehabilitative, and nutritional care to over 175,000 children and young adults in fifteen countries. Our singular goal is to provide free care to children with severe congenital facial deformities, tumors of the face and neck, burn injures, dental disease, and malnutrition. The children we are privileged to serve live in the most impoverished corners of the world, and without the commitment of our volunteers, and the generosity of our benefactors, these children would continue to live without any hope of receiving the surgical, dental, and medical care they so desperately need.
Lack of essential hospital infrastructure in Rwanda, Tanzania, and Ukraine necessitated a build-out of operating room facilities prior to the initiation of charity missions in each of these countries. In Tanzania and Rwanda, MMFC installed anesthesia machines, operating room tables and overhead lighting, vital surgical equipment, and state-of-the-art operating room and post-op recovery room monitors at hospitals in Dar es Salaam and Gitwe, respectively. MMFC similarly outfitted three hospitals in Ukraine, with a modern microvascular surgical laboratory assembled at a regional burn center in the city of L’viv. These donations, along with the training of local physicians by MMFC volunteer surgeons and anesthesia staff, allow these medical facilities to extend their scope of care 52 weeks a year.
By way of partnership with the Maharlika Charity Foundation, MMFC has been able to reach destitute communities throughout the Philippines—on the islands of Luzon, Samar, Leyte, Palawan, and at multiple sites in Mindanao. At two separate sites in the Philippines—Angeles City and Davao City—MMFC and Maharlika, working hand in hand, are developing cleft care centers that will provide surgical, rehabilitative, and/or nutritional care twelve months a year.
What We Do


Cleft Lip & Cleft Palate
Out of the twenty children who are born every hour with a cleft lip and/or cleft palate, nineteen live in a country that has no capacity to care for them. The African nation of Tanzania, with a population of 67 million people and a land mass twice the size of California, highlights the desperation that these children face. We have been sending surgical teams to Dar es Salaam, Tanzania, for over 25 years, where we operate on children at the one hospital in the entire country that cares for patients with cleft deformities. There, we work hand in hand with the only three doctors in all of Tanzania who are trained in cleft care.
Without surgical and rehabilitative therapy, children suffering from a cleft deformity face a life of unimaginable difficulties in regards to breathing, speaking, nutrition, hearing, and their mental health. Growth and development can be severely impaired, and respiratory infections are far more frequent in children with an unrepaired cleft. Social isolation is an unavoidable reality for almost all affected children, and not infrequently, a child with a severe facial deformity is abandoned and orphaned.
But no matter how extreme the deformity, a child born with a cleft lip and/or cleft palate can, in many ways, be made whole.
Ideally, surgical repair of a cleft lip is completed during the first year of life. However, as evident in the photos below, no age is “too old” to repair such an extreme deformity. A cleft of the palate can be repaired between eighteen months and ten years of age, and throughout this process, every child undergoes multiple stages of dental care, speech and language therapy, and nutritional care. Between the ages of ten and eighteen years, our patients undergo bone grafting to repair the upper jawbone and, if indicated, surgery to improve the nasal air passage.



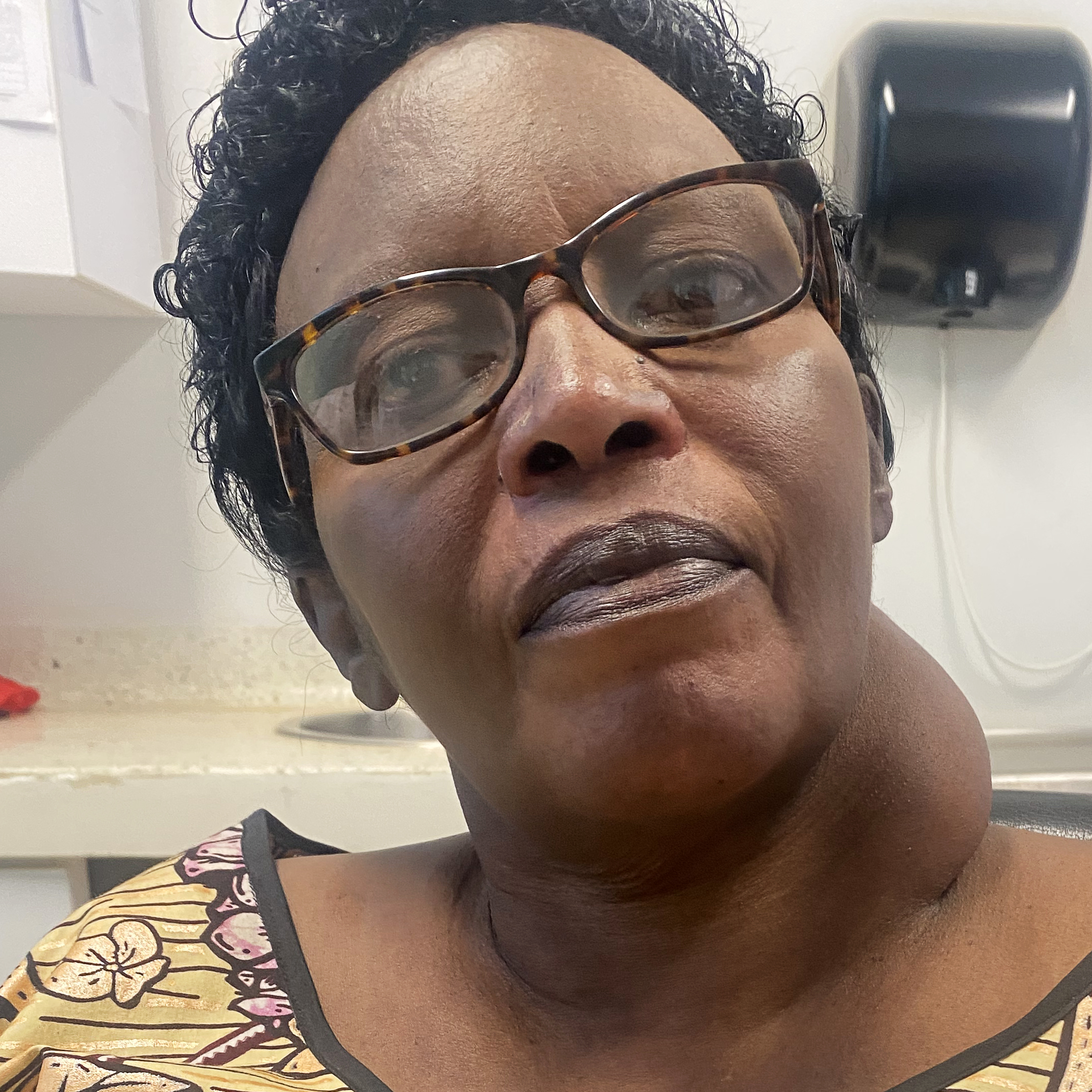
Thyroid
In Africa and parts of Asia, overgrowth of the thyroid gland, commonly known as a giant goiter, is caused by dietary iodine deficiency. After many years of working with MMFC teams in caring for children with cleft deformities, medical professionals in Rwanda and the Philippines requested our help in treating the overwhelming population of patents with untreated giant goiter. Due to the lack of medical services in these countries, patients affected by giant goiter generally come to medical attention at a late stage of the disease, when the enlarged gland compresses the windpipe and esophagus and causes symptoms such as shortness of breath, neck and throat tightness, difficulty swallowing, hoarseness, and chronic cough. A giant thyroid goiter is shockingly evident to everyone the affected patient encounters, and with time, such growths cause restricted neck mobility and marked impairment of a normal sleep pattern due to airway pressure.
Surgical removal of a giant goiter is a one-stage operation that takes no more than two hours to complete. Fortunately, the vast majority of goiters are non-cancerous. After surgery, all patients are placed on thyroid and calcium replacement therapy, with regular follow-up and blood testing by our physician colleagues on-site.

Microtia
Microtia, or absence of a normal outer ear, is a rare but devastating congenital deformity. A microtia deformity occurs during the first weeks of an expectant mother’s pregnancy, and while there are known genetic components, research suggests various environmental factors, including maternal use of alcohol and tobacco. While microtia can be associated with a number of known syndromes, many afflicted children in Central America, and in the Andean cultures of Ecuador and Peru, are otherwise healthy.
Microtia repair is a three stage process that begins no earlier than a child’s seventh birthday. The first stage involves the harvesting of a small section of the child’s rib cartilage, which is then sculpted into the structural anatomy of a normal ear. This cartilage graft is then immediately implanted into the anatomically proper level, deep to the scalp skin on the affected side. The second stage, completed six to twelve months later, involves “bringing out” the previously implanted graft, with the covering of any raw surface by way of a skin graft(note: skin grafts are generally harvested from the upper thigh, with no visible scar left behind). Last, the ear lobe is created by rotating healthy skin ninety degrees into the lower part of the previously sculpted graft tissue.


Burn Care
Every day, 30,000 people suffer a severe burn injury, with 70% of these injures occurring in the impoverished countries of sub-Saharan Africa and Southeast Asia. The causes of these horrific injures in the underdeveloped world are many, including:
- Open fires as a source of heat and cooking.
- Faulty electrical wiring with lax, and often non-existent, building codes.
- Improperly stored chemicals and petroleum products.
- No access to flame resistant clothing.
- Exposed vats of boiling water over an open flame outside the home.
Burn prevention measures have no traction within these destitute communities, and major limitations to burn care management include a lack of appropriately trained staff, and absence of the equipment and resources necessary for long-term wound care. MMFC physicians and nurses have worked hand in hand with local professionals in Tanzania, India, and Rwanda, providing chronic burn wound care to children and young adults at multiple facilities. From 1998 through 2021, MMFC sent over sixty such teams to Ukraine, working with the thoroughly dedicated staff at the regional pediatric burn center in L’viv. In addition to caring for over 7000 Ukrainian citizens, MMFC built out a fully equipped operating room suite and microvascular lab. By way of the training provided by a member of the MMFC surgical team, our Ukrainian colleagues began utilizing state-of-the-art techniques in treating life-threatening burn wounds.


Dental Care
The complexity of dental disease in children born with a cleft deformity cannot be overstated. Infectious complications from chronic, untreated dental disease can be life-threatening, and children with cleft lip and palate are at particularly high risk due to:
- Multiple misplaced teeth.
- Missing teeth on one side of the upper jawline, with extra teeth on the opposite side. -deeply impacted dental roots.
- Severely twisted and misaligned teeth.
- Infected teeth within the sinus tissue.
- Delayed dental eruption.
- Crown and root malformation.
- Multiple decaying teeth.
Since MMFC’s first international mission in 1991, dental care has been an integral part of each mission site in every country we visit. Dental care begins in infancy and continues indefinitely, and includes:
- Full evaluation at the time of cleft lip repair.
- Providing soft toothbrushes and toothpaste to every child.
- Restoration of primary and secondary teeth whenever possible. Should there be no other viable option, limited dental extractions are performed.
- Treatment of dental cavities.
- Employing bridges, implants, and crowns whenever possible.
- Fitting for an oral prostheses to address missing teeth and/or gaps within the front portion of the palate.
- Orthodontic therapy at some mission sites.
- Bone grafting at age 9-12 in order to bring the upper gum line together.

Nutritional Program
Currently, MMFC carries out missions at 23 separate sites in eleven countries, and a grim reality that children at each of these sites face is chronic malnutrition. According to the Institute for Health Metrics and Evaluation(IHME), a Seattle-based independent health research organization, children with cleft deformities are twice as likely to be malnourished than are otherwise healthy children. Without early intervention, a child born with a cleft lip and/or cleft palate will fall further and further behind on the growth curve, resulting in a weakened immune system. Immunocompromised children are at higher risk for wound complications after corrective surgery, and more prone to potentially life-threatening respiratory infections. IHME estimates that nearly half of all malnutrition-related deaths in children with cleft conditions could be prevented by way of access to adequate nutritional therapy. In January 2024, MMFC received funding to develop a Nutritional Support Program at our mission sites in Guatemala. This allowed us to provide vital nutritional supplementation to the children we care for, along with an educational program to assist each child’s caregiver. Our goal is to expand this program into every site MMFC serves in Asia, East Africa, and Latin America. While the Nutritional Support Program has to date been immensely successful, our vision for its growth—treating between 3000 and 4000 desperately poor children every year— can only happen by way of your generosity, and the commitment of our dedicated volunteers around the world. Please, help us help them.

